Charlie
Pediatric Post-Hospitalization Patient Portal for Children’s Hospital of Pittsburgh
Team: Rayna Allonce, Felix Liu, Neha Agarwal, Marty Bacik, Megan Conover
Role: UX Researcher & Product Designer
Timeline: 24 Hours, October 2018
UX Research, UX/UI Design, MedTech
4th Place Winner of "Hack This. Help Kids." Healthcare Hackathon
Overview
In a 24 hour pediatric health hackathon my team researched, designed, and presented a prototype of a solution that both improves the post-hospitalization planning process for parents and caregivers at the UPMC Children’s Hospital and engages and empowers young patients in the management of their care.
Our design process primarily included a deep dive into our problem area. We spent about half of our working time talking to over 15 different physicians, nurses, hospital administrators, and patients to better understand the problem. Following our research we went broad and ideated various concepts, then narrowed in on a single solution and iterated and tested our concepts with stakeholders. To ground our design we focused on the single use-case of a patient with diabetes.
THE PROBLEM
How might we design an effective system for providing patient families with post-discharge care instructions that properly educates families upon a patient’s discharge to help ensure a healthier child and avoid re-admissions to the hospital?
When patients are ready to go home from the hospital, the clinical education specialists at UPMC Children’s educate the families on discharge instructions. This includes scheduling follow-up appointments, reviewing medications that are to be taken at home, and general education on the patient’s path to recovery. This education is often verbal, with patients being given a thick packet of discharge documents as well to refer back to.
However, although caregivers and patients are given a lot of information in the moments leading up to discharge, this vital information may be miscommunicated or unintentionally ignored, endangering the patient’s wellbeing.
Readmission is not only costly to the health and wellbeing of the patient, but to the hospital and the healthcare system at large.
THE SOLUTION
An online portal that structures the physical post-hospitalization plan documents in an easily digestible format and incorporates a tamogachi-like virtual simulation that mimics the condition and treatment plan of the patient
We leveraged and structured already existing data (here the tangible discharge documents received by all patient families) and placed it on digital health management platform accessible by QR code. Embedded in the platform is Charlie, a tamogachi-like virtual simulation that mimics the condition and treatment plan of the patient. In learning how to take care of Charlie, pediatric patients are empowered to learn how to better take care of themselves.
Feature 1: QR code on already existing physical document leads to an online portal
Instead of reinventing the wheel, with the addition of a QR code on the physical post-hospitalization plan documents already handed out to patients, we propose structuring the data in an online dashboard. This information is structured in an easily digestible format and give parents easy access to the information at any time. As a result, they can look at it when they are more willing and able to digest.
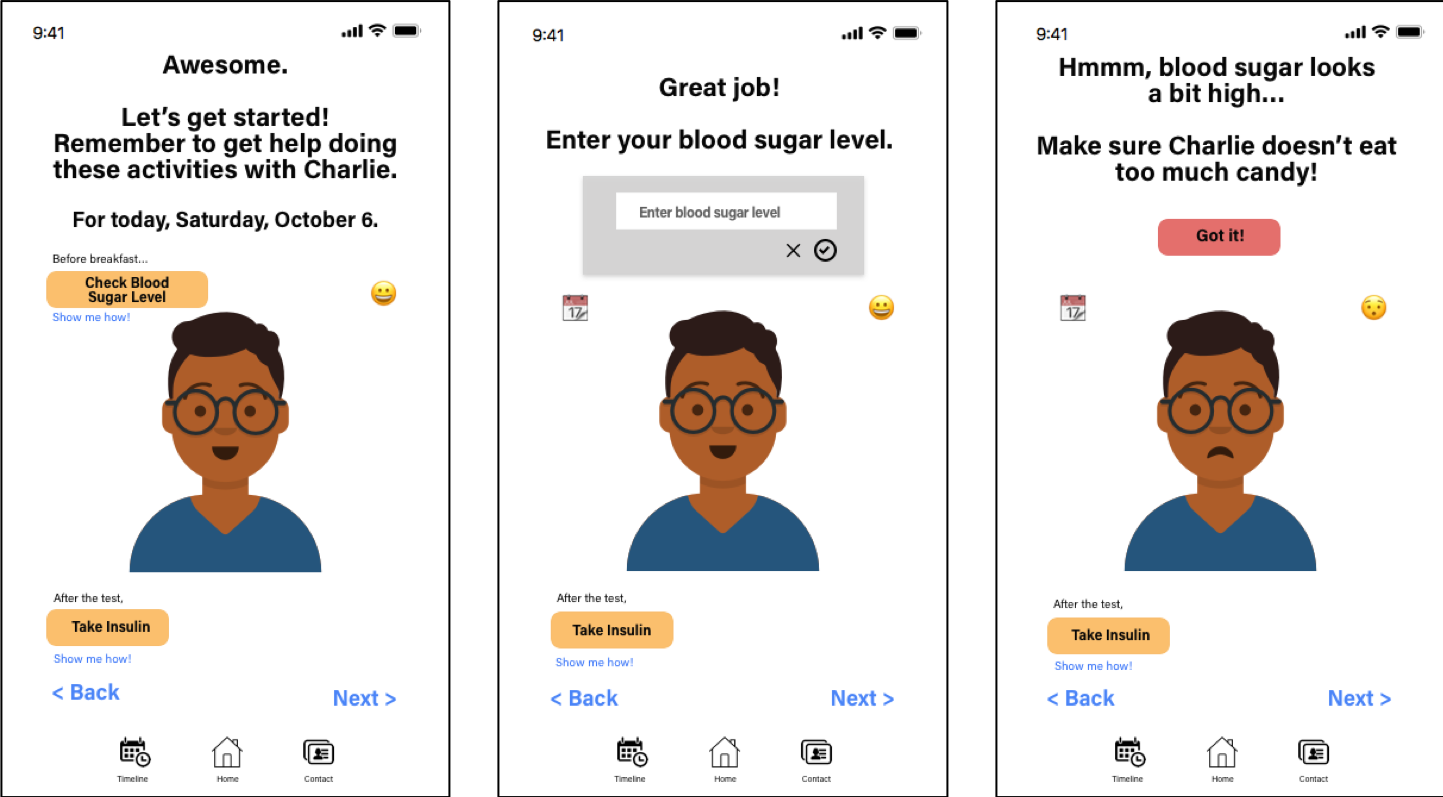
Feature 2: Charlie, a tamogachi-like virtual simulation
Our “secret-sauce” was the integration of a virtual simulation we named Charlie (meant to be gender-neutral), that mimics the condition and treatment plan of the patient. We not only wanted to help parents and caregivers better take care of their children, but also empower our patients to take care of themselves, and how better to teach them than to teach them how to take care of someone else.
The avatar is a way for us to facilitate education from the very start, without increasing burden for our nurses. The patient can create their avatar while the nurse explains post-hospitalization to parents, increasing literacy from the very start. Once at home, patients can continue to take care of Charlie, with the help of an adult for younger children.
Charlie’s cartoon-like visual design is meant to make the experience less scary and confusing for young patients. The avatar mimics the patient and is meant to humanize the experience (for example, it is scared of finger pricks). We wanted to give young patients the feeling that “I can do this! Even though it’s hard.”
IMPACT AND FUTURE OPPORTUNITIES
Charlie can serve as a foundation to future work
Our solution was widely regarded by judges and stakeholders as being easily implementable and innovative. It fits into the existing system, engages both patients and caregivers, and sets a foundation for the future. In future iterations we imagine that Charlie can be leveraged for:
Social avatar networks
Presenting research opportunities
Information tracking and sharing between patients and healthcare providers
Tailoring learning experiences
Measuring health literacy